Mobility
The consequences of immobility are wide-ranging and can have far-reaching detrimental effects for patients and their families. Caregivers struggle to provide mobility activities for their patients due to workload, patient condition and fear of an unsafe event. This section provides the latest evidence-based recommendations for safely mobilizing patients, including overviews of the literature that support mobility safety.
The Body at Rest: The Consequences of Immobility
The intended audience for this course is nurses whose practice includes the care of patients with any mobility issues.
Learning objectives
- Describe the effects of immobility on the body's systems
- Describe the major conditions caused by immobility
- Name the potential hospital-acquired conditions which improved mobility may help prevent
Everyday Mobility
Learning objectives
- Challenges of mobility
- Complications of immobility
- Benefits of mobility
- Clinical recommendations
- Mobility resources
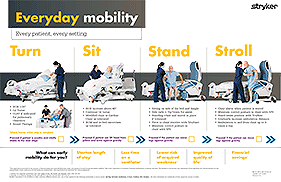
Everyday Mobility Card
Every patient, every setting.
This algorithm is provided for the purpose of demonstrating how Early Mobility may assist with physical reconditioning and patient mobility.
Fast Track to Early Mobility
Stryker’s prevention policy is product + process = prevention. As part of that philosophy, we have created our early mobility program to help caregivers reduce the complications of immobility. Our program provides systematic means to educate staff on looking closely at existing policies and standards of care, update patient safety supported by evidence, and utilize hospital equipment to help nursing and ancillary staff in their efforts to keep patients safe and comply with facility policies.
Society of Critical Care Medicine: ABCDEF Bundles
ICU Liberation: ABCDEF Bundles
The ABCDEF Bundle elements individually and collectively can help reduce delirium, improve pain management and reduce long-term consequences for adult intensive care unit (ICU) patients.
Enhancing Compliance to the Seated Portion of a Hospital Mobility Bundle: A Mixed Method Case Study
Author: Christopher Kowal DNP, RN
To characterize nursing perceptions and attitudes through description of consistent themes following the pilot of a new type of Seated Positioning System (SPS) device in care of the out of bed (OOB), seated patient.
Seated patients become a safety risk for personal injury due to: (a) risk for falls from transferring, slouching, or upright sitting compliance; (b) chair-slouching that could lead to difficulties in breathing and swallowing; and (c) noncompliance in following safety protocols when sitting OOB.
Helping Nurses Achieve the Objectives for Early Mobility
Author: Guy Fragala Ph.D., PE, CSP, CSPHP
Instituting a planned, structured ICU early mobility quality improvement project can result in improved outcomes and reduced costs for ICU patients across healthcare systems, (Engel 2013). A financial model was developed using data from existing studies and from the actual implementation of early mobilization in the MICU at Johns Hopkins Hospital. Data from this study of early mobilization in the ICU indicated a 22% reduction in stay with an average of 5.4 days before intervention and 3.9 days post intervention, (Lord et al 2013).
Based on an analysis of data from prior publications and the early rehabilitation program in the Johns Hopkins Medical ICU, the report authors developed a conservative model for net financial savings and costs. This analysis demonstrated that most ICUs with between 200 and 2000 annual admissions would generate a net savings of up to 3.76 million dollars by reducing patient ICU length of stays (Lord et al 2013).
Innovative Seated Positioning Device: Improves Safe Patient Handling While Reducing Risk Factors for Pressure Ulcers and Falls
Author: Craig Golden, MPT
HCWs using the seated positioning system felt the product was better than current standard of care for helping to reduce risk factors for pressure ulcers, patient falls, and injury, mitigating several issues associated with patients in bedside chairs.
Specifically, HCWs felt the product helped minimize downward migration, thus reducing the potential for friction and shear forces on the skin – two key risk factors for pressure ulcers. In addition, HCWs felt the product helped reduce patient fall risk as the patient was less likely to slide down the chair and onto the floor. Finally, HCWs felt the device made it easier to move and position patients with less physical effort, thus reducing the risk of musculoskeletal injury.
Early Mobility Program Results in Improved Patient Outcomes and Cost Savings
Authors: Lilia Hansen, MSN, MBA, RN, CCRN, Sarah Malcom MSN, RN, Heidi Brooks MSN APRN-FNP
An intensive care unit (ICU) at Nebraska Methodist Hospital implemented an early mobility program to enhance patient safety in their clinical environment.
The following case history outlines their efforts and the results of their quality improvement (QI) initiative.
28996