Mako Total Knee 2.0
The next chapter of SmartRoboticsTM
Informed by over 500,000 Mako Total Knee procedures over the past six years, Mako Total Knee 2.0 is designed to deliver the same trusted outcomes surgeons expect from Mako with a new, elevated user experience they deserve.
Unleash the future
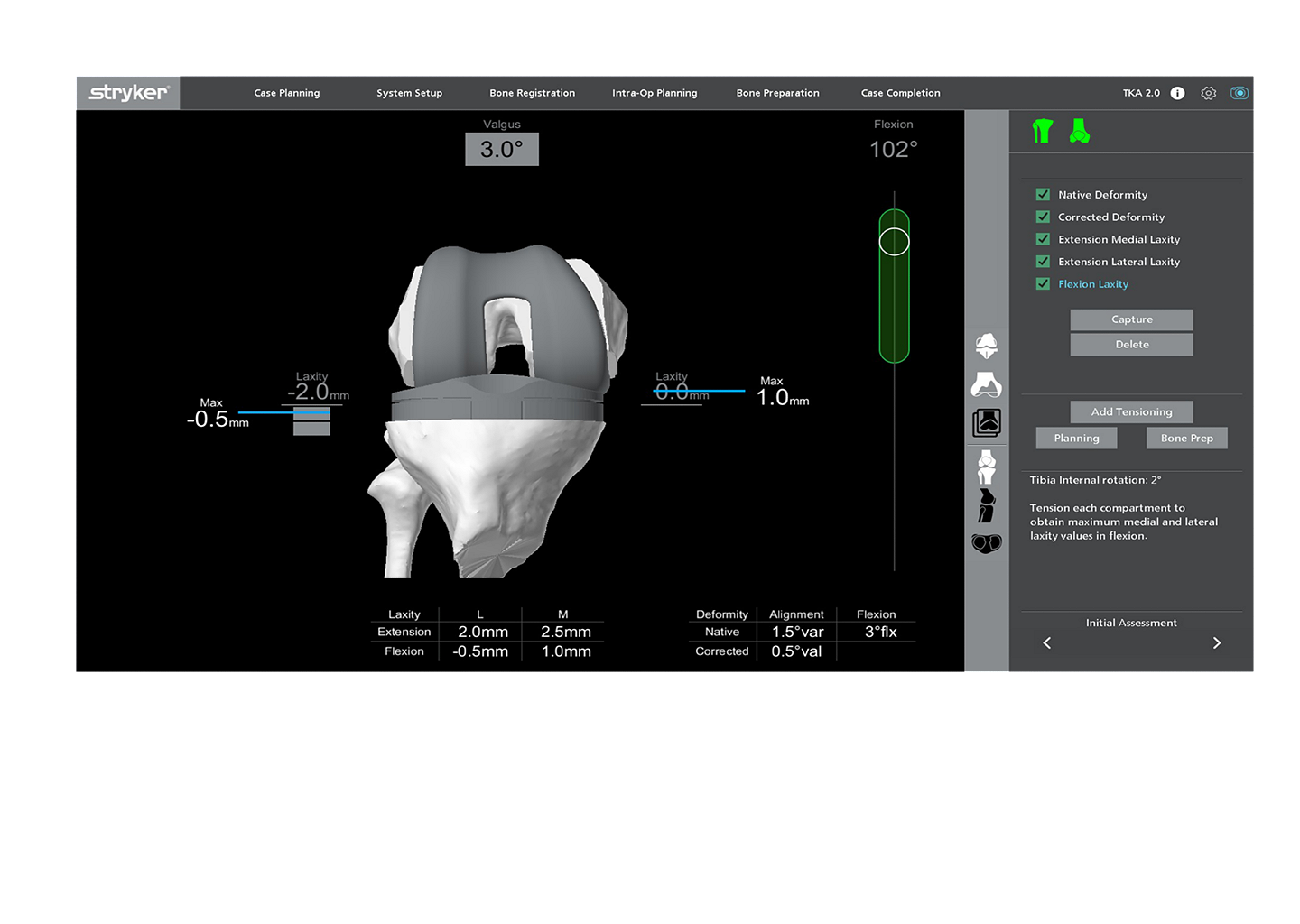
Mako Total Knee 2.0 drives ease of use through its intuitive design, a customizable step-by-step workflow and innovative features – including a digital tensioner that allows surgeons to assess the knee’s stability intraoperatively during a total knee arthroplasty (TKA) without any additional instrumentation.
There’s often a perception that robotics is complex and can be intimidating, which is why we are so excited about this launch – it delivers an unparalleled robotic experience.
Confidence and control
Customizable workflow based on surgeon preferences with increased surgeon control.
Confidence and control
Intuitive, step-wise approach that allows you to navigate the procedure with ease.
Functional Knee Positioning™
Ability to acknowledge proxies for knee function, based on each patient’s bony anatomy, with the execution of AccuStop™ haptics.
Surgical efficiencies
Streamlined surgical workflow to enable surgical efficiencies throughout the entire procedure.
Mako Total Knee 2.0 features a new Digital Tensioner
- Standard soft tissue balancing techniques utilized in total knee arthroplasty (TKA) can often be subjective, centered around a surgeon’s feel of ligament laxity.1
- The Mako Total Knee 2.0 digital tensioner has demonstrated excellent repeatable ligament laxity assessments and reproducible ligament assessments within 1mm.2
- No additional instrumentation or hardware
- Audible and visual guidance provided to the surgeon during assessment, every 0.5mm
**Data on file. Stryker’s internal sales data, 2022.

Mako Total Knee 2.0 is focused on enhancing the surgeon experience, driving efficiencies and increasing surgeon confidence.
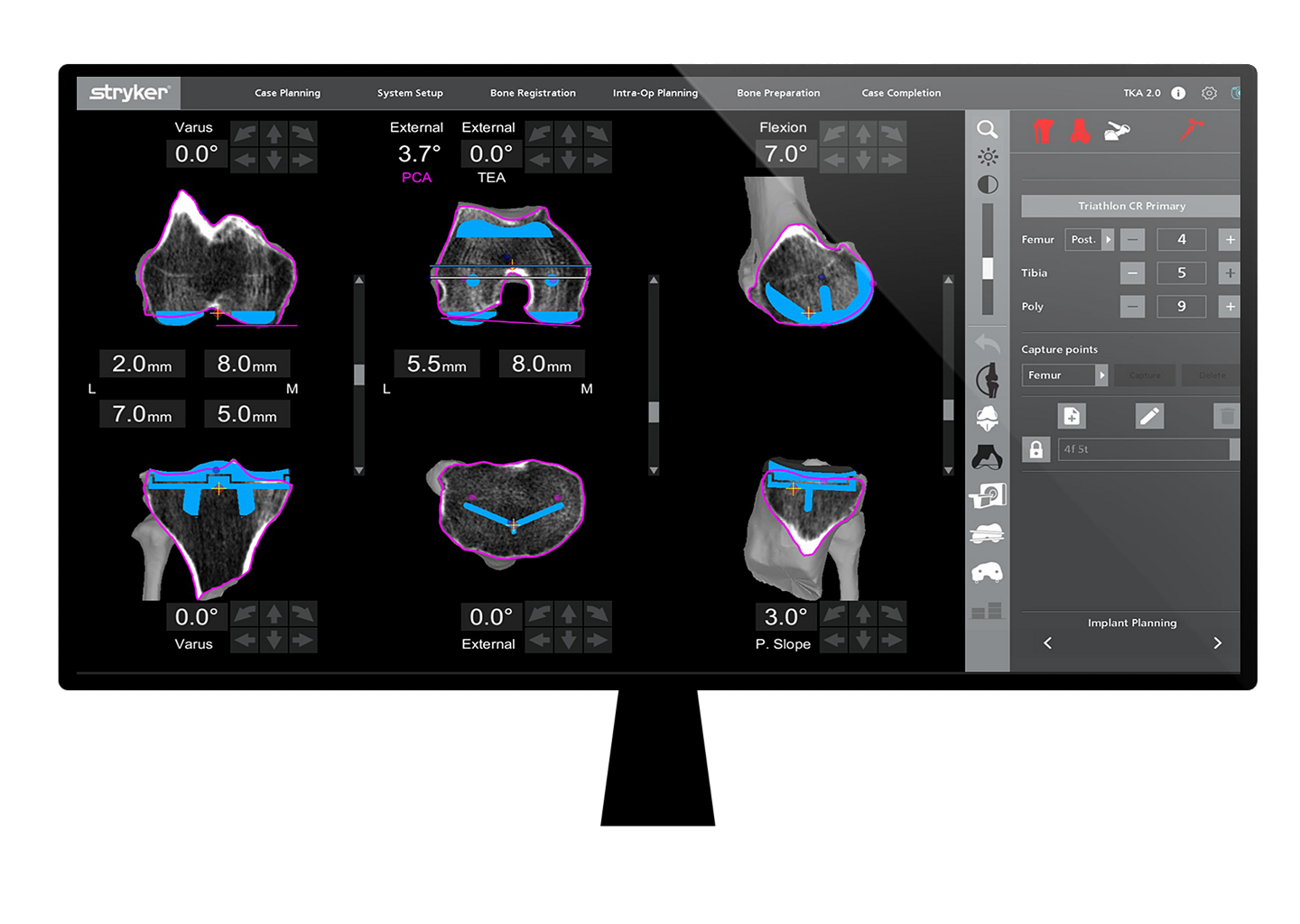
Greater precision to plan
Studies have shown 3D CT planning and haptic boundaries allow surgeons to deliver a more precise procedure,6 with less soft tissue damage compared to manual.4,7
Less pain, fewer meds
Patients experienced less pain,3 and required less pain relief8 compared to manual total knee replacement.
Improved early recovery
In the Australian Registry, four-year survivorship of the Triathlon CR implanted with Mako had a relative improvement of 19% over manual TKA.10
Improved mid-term survivorship
A cadaveric study has shown that registration landmarks are more accurately identified using a 3D CT scan compared to intra-op points captured manually.12
Surgeon confidence
95% of users surveyed reported overall increased confidence intraoperatively compared to manual total knee.11
Intuitive design
84% of users surveyed reported intuitive use of the system.11
New Digital Tensioner
A cadaveric study has shown excellent repeatable ligament laxity assessments and reproducible ligament assessments within 1mm.2
Accurate 3D CT registration
A cadaveric study has shown that registration landmarks are more accurately identified using a 3D CT scan compared to intra-op points captured manually.12
"Mako Total Knee with the new 2.0 software offers an intuitive workflow that simplifies my ability to perform patient specific functional implant positioning. An added bonus are the new features that make bone cutting and preparation highly efficient. The planning and execution makes this the ideal tool for me to perform TKA’s efficiently in my ASC.”
—Joseph Nessler, M.D.
Dr. Nessler is a paid consultant of Stryker Orthopaedics. The opinions expressed by Dr. Nessler are those of Dr. Nessler and not necessarily those of Stryker. Individual experiences may vary.
"Mako Total Knee 2.0 is intuitive, accurate to plan, and efficient. It provides me with increased surgeon autonomy while also allowing me to have a unique customizable experience. What more could I ask for?”
—Paul Jacob, D.O.
Dr. Jacob is a paid consultant of Stryker Orthopaedics. The opinions expressed by Dr. Jacob are those of Dr. Jacob and not necessarily those of Stryker. Individual experiences may vary.
Contact us
Send us a message to learn more about Mako Total Knee 2.0
This contact form is intended for healthcare professionals. If you’re looking to contact us about patient materials, please go here.
*For the Mako Total Knee application, “cut less” refers to less soft tissue damage and greater bone preservation as compared to manual surgery.4,5
- Kwak DS, Kong CG, Han SH, Kim DH, In Y. Development of a pneumatic tensioning device for gap measurement during total knee arthroplasty. Clin Orthop Surg. 2012;4(3):188-192. doi:10.4055/cios.2012.4.3.188
- Scholl L, Caba M, Hampp E, Ali A, Crutcher J, Mont M, Mahoney O: Robotic-assisted total knee arthroplasty technology helps provide a repeatable and reproducible method of assessing soft tissue balance. Poster 1683. Orthopaedic Research Society 2023 Annual Meeting; February 10-14; Dallas Texas.
- Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J. 2018;100-B(7):930-937. doi:10.1302/0301-620X.100B7.BJJ-2017-1449.R1
- Kayani B, Konan S, Pietrzak JRT, Haddad FS. Iatrogenic Bone and Soft Tissue Trauma in Robotic-Arm Assisted Total Knee Arthroplasty Compared With Conventional Jig-Based Total Knee Arthroplasty: A Prospective Cohort Study and Validation of a New Classification System. J Arthroplasty. 2018;33(8):2496-2501. doi:10.1016/j.arth.2018.03.042
- Hozack WJ. Multicentre analysis of outcomes after robotic-arm assisted total knee arthroplasty. Bone Joint J:Orthop Proc. 2018;100-B(Supp_12):38.
- Deckey DG, Rosenow CS, Verhey JT, et al. Robotic-assisted total knee arthroplasty improves accuracy and precision compared to conventional techniques. Bone Joint J. 2021;103-B(6 Supple A):74-80. doi:10.1302/0301-620X.103B6.BJJ-2020-2003.R1
- Fontalis A, Kayani B, Asokan A, et al. Inflammatory Response in Robotic-Arm-Assisted Versus Conventional Jig-Based TKA and the Correlation with Early Functional Outcomes: Results of a Prospective Randomized Controlled Trial. J Bone Joint Surg Am. 2022;104(21):1905-1914. doi:10.2106/JBJS.22.00167
- Bhimani SJ, Bhimani R, Smith A, Eccles C, Smith L, Malkani A. Robotic-assisted total knee arthroplasty demonstrates decreased postoperative pain and opioid usage compared to conventional total knee arthroplasty. Bone Jt Open. 2020;1(2):8-12. Published 2020 Oct 27. doi:10.1302/2633-1462.12.BJO-2019-0004.R1
- Marchand RC, Scholl L, Taylor KB, et al. Clinical Outcomes after Computed Tomography-Based Total Knee Arthroplasty: A Minimum 3-Year Analyses [published online ahead of print, 2023 Jan 19]. J Knee Surg. 2023;10.1055/s-0042-1759790. doi:10.1055/s-0042-1759790
- Australian Orthopaedic Association National Joint Replacement Registry. Hip, Knee & Shoulder Arthroplasty 2022 ANNUAL REPORT. [Available at https://aoanjrr.sahmri.com/annual-reports-2022].
- Valentino A, Scholl L, Caba M, Hampp E, Mont M, Mahoney O: Assessing Surgeon Confidence and Efficiencies when Utilizing Robotic Assisted Total Knee Arthroplasty. Poster 1680. Orthopaedic Research Society 2023 Annual Meeting; February 10-14; Dallas Texas.
- Chen A, Caba M, Ali A, Crutcher J, Mont M, Mahoney M: What is the best way to identify the transepicondylar axis for femoral component rotation? Poster 0855. Orthopaedic Research Society 2023 Annual Meeting; February 10-14; Dallas Texas.
JR-MTKA-SYK-666320



