SPY-PHI
SPY Portable Handheld Imaging System
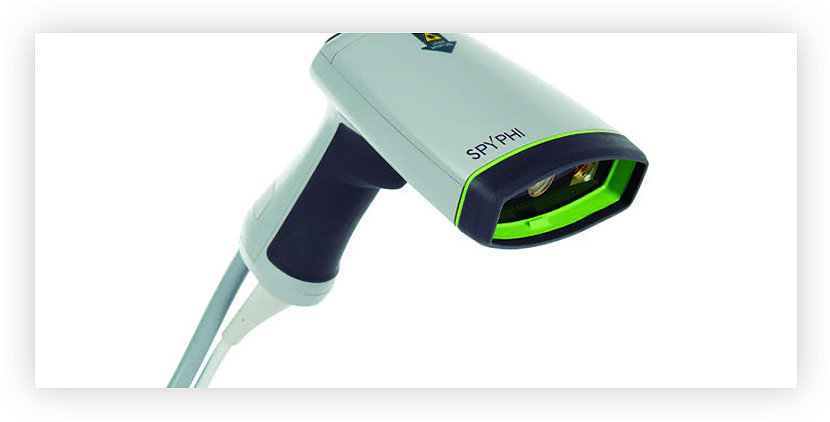
Indications for use
The SPY Portable Handheld Imaging System (SPY-PHI System) is an active device used to visualize circulation, including lymphatics and blood vessels, as well as related tissue perfusion with near infrared fluorescence imaging during a variety of surgical procedures.
1688 AIM
4K Camera System

Indications for use
The 1688 Advanced Imaging Modalities (AIM) 4K platform enables surgeons to perform minimally invasive surgery using standard endoscope visual light as well as visual assessment of vessels and microvessels, blood flow and related tissue and organ perfusion, lymphatics, perfusion associated with tumors and tumor margins, and at least one of the extra-hepatic bile ducts (cystic duct, common bile duct and common hepatic duct) using near-infrared imaging.

Is fluorescence guided surgery as effective as other tracers in sentinel lymph node (SLN) detection in breast cancer patients?
Fluorescence guided SLN biopsy in breast cancer patients is not inferior to the RI+BD technique or to RI alone.
- Ballardini et al. (2013) included n = 134 woman in a prospective study and assessed concordance between the ICG method and the 99mTc method. Authors concluded that the ICG method is not inferior to that of RI and can be used alone to reliably identify SLNs.
- In a prospective study, Samorani et al. (2015) aimed to validate the ICG method of detecting SLN in breast cancer patients. Authors enrolled n = 301 patients who underwent SLN detection using both the 99mTc – and the ICG method. 99% of the nodes were identified with ICG, and 76.7 % were identified with 99mTc.
- Somashekbar et al. (2020) conducted a prospective, comparative study to assess the detection and accuracy of SLN detection with ICG in comparison to the dual-dye technique (RI+BD). SLN detection was performed in n = 100 patients, the identification rate with the dual dye technique was 94%, whereas with ICG alone, it was 96%.
- In a meta-analysis, Kedrzycki et al. (2021) demonstrated the ICG is equivalent to RI in node identification. This finding was based on n = 944 patients out of 10 studies.
Fluorescence guided SLN biopsy in breast cancer patients is not inferior to the RI+BD technique or to RI alone.
- Ballardiniet al. (2013) included n = 134 woman in a prospective study and assessed concordance between the ICG method and the 99mTc method. Authors concluded that the ICG method is not inferior to that of RI and can be used alone to reliably identify SLNs.
- In a prospective study, Samoraniet al. (2015) aimed to validate the ICG method of detecting SLN in breast cancer patients. Authors enrolled n = 301 patients who underwent SLN detection using both the 99mTc –and the ICG method. 99% of the nodes were identified with ICG, and 76.7 % were identified with 99mTc.
- Somashekbaret al. (2020) conducted a prospective, comparative study to assess the detection and accuracy of SLN detection with ICG in comparison to the dual-dye technique (RI+BD). SLN detection was performed in n = 100 patients, the identification rate with the dual dye technique was 94%, whereas with ICG alone, it was 96%.
- In a meta-analysis, Kedrzyckiet al. (2021) demonstrated the ICG is equivalent to RI in node identification. This finding was based on n = 944 patients out of 10 studies.
Note - 1688 AIM is not indicated for lymphatic mapping in breast surgery
Is fluorescence guided surgery as effective as other tracers in sentinel lymph node detection in cervical cancer patients?
ICG FA has a higher SLN bilateral detection rates than 99mTc + BD.
- Beaten et al. (2021) included a meta-analysis on 589 patients out of 7 studies and concluded that ICG appears to result in higher bilateral SLN detection compared to the combination of 99mTc + BD.
- Buda et al. (2016) included 114 women with cervical cancer into a retrospective study, comparing SLN detection rates of ICG vs RI+BD. Bilateral mapping was achieved in 98.5% for ICG and 76.3% for 99mTc + BD.
- Buda et al. (2018) performed another retrospective study and included 65 women with early-stage cervical cancer. The authors compared bilateral SLN detection rates of ICG vs 99mTc + BD (95.2% vs 69.6%).
- Di Martino et al. (2017) conducted a retrospective multi-center study and assessed 95 women with stage IB1 cervical cancer. 47 patients underwent SLN mapping with 99mTc +/-BD and 48 with ICG. A 91.7% bilateral SLN detection rate was achieved with ICG, compared to 66% obtained with 99mTc.
Is fluorescence guided surgery a useful tool to reduce post-operative complications after colorectal cancer surgery?
ICG-FA can reduce the risk for anastomotic leaks after colorectal cancer surgery.
- Alekseev et al. (2020) demonstrated in a single-center RCT (n=380 pts) a significant reduction of AL rates in LAR from 25.7% in the non-ICG-FA group to 14.4% in the ICG-FA group.
- In a retrospective comparative study, Ishii et al. (2020) found that the AL rate was significantly lower in the ICG group (1.8%) compared to the non-ICG group (5.3%) for rectal cancer patients.
- Kim et al. (2016) performed a cohort study of 436 rectal cancer patients, demonstrating a significant reduction of AL in the ICG group (0.8 % vs 5.4%).
- In a series of 50 patients, Skrovinaet al. (2020) found a significant reduction of AL in the ICG-FA group (10%) when compared to a historical control without ICG-FA (18%).
- Wada et al (2019) performed a retrospective PSM study of 149 patients and detected a reduction in symptomatic AL rate from 14.7% (no ICG) to 8.8% (ICG-FA)
- In a retrospective study, Mizrahi et al. (2018) compared AL rates of patients who underwent LAR and observed a reduction of AL rate from 6.7% (no-ICG group) to 0% (ICG-FA group).
- Wanatabeet al. (2019) found a significantly reduced AL rate in a retrospective PSM cohort study (OR 0.427, CI 0.197 –0.926)
ICG-FA can reduce the risk for re-operation after rectal cancer surgery.
- Wanatabe et al. (2019) performed a multi-center, retrospective PSM study and found a significantly lower rate of re-operations in the ICG-FA group (OR 0.19, CI 0.042 – 0.889).
- In a retrospective case-control analysis, Jafari et al (2013) found a reduction of the re-operation rate from 9% to 6% for non-ICG and ICG, respectively.
ICG-FA can reduce length of hospital stay.
- In a retrospective PSM study, Wanatabe et al. (2019) found a significantly shorter post-operative hospital stay in the ICG-FA group: x (mean) = 2.62 days, (CI 0.96 – 4.28).
ICG-FA can reduce operative time.
- In a retrospective study of n=657 rectal cancer patients Kim et al. (2017) found significant difference in OR time from between ICG-FA (177 ± 43 min) and no-ICG-FA group (197 ± 47 min)
Stryker´s fluorescence imaging system requires the imaging agent Indocyanine Green (ICG). Indocyanine green (ICG) is a drug and is not provided by Stryker but is independently sourced by the customer. The approval status of the drug may vary. Customers shall determine the status applicable at their hospital in their country and consult the manufacturer’s instructions of the drug for specifications and use.

Associate Prof. Dr. med. Mustafa Muallem
Germany
Deputy Director of the Department of Gynecology with Center for Oncological Surgery, Charité Medical University of Berlin
Mr. John Butler
United Kingdom
Consultant Gynaecologist and Gynaecological Oncology Surgeon
Royal Marsden Hospital
Professor Dawid Murawa
Poland
Surgical Oncology Specialist
Head of the Oncological Surgery Clinic, Zielona Góra University Hospital

Copyright © 2019 Stryker. Stryker Corporation or its affiliates own, use or have applied for the following trademarks or service marks: Stryker, SPY, SPY-PHI, Iris and Pneumoclear. All other trademarks are trademarks of their respective owners or holders.
Colorectal
- Alekseev, M., Rybakov, E., Shelygin, Y., Chernyshov, S. & Zarodnyuk, I. A study investigating the perfusion of colorectal anastomoses using fluorescence angiography: results of the FLAG randomized trial. Colorectal Dis 22, 1147–1153 (2020).
- Ishii, M. et al. Efficacy of indocyanine green fluorescence angiography in preventing anastomotic leakage after laparoscopic colorectal cancer surgery. Int J Colorectal Dis 35, 269–275 (2020).
- Kim, J. C., Lee, J. L., Yoon, Y. S., Alotaibi, A. M. & Kim, J. Utility of indocyanine-green fluorescent imaging during robot-assisted sphincter-saving surgery on rectal cancer patients: Indocyanine green in robot surgery. Int J Med Robotics ComputAssist Surg 12, 710–717 (2016).
- Mizrahi, I. et al. Indocyanine green fluorescence angiography during low anterior resection for low rectal cancer: results of a comparative cohort study. Tech Coloproctol22, 535–540 (2018).
- Skrovina, M. et al. The significance of intraoperative fluorescence angiography in miniinvasivelow rectal resections. wiitm15, 43–48 (2020).
- Wada, T. et al. The effects of intraoperative ICG fluorescence angiography in laparoscopic low anterior resection: a propensity score-matched study. Int J Clin Oncol 24, 394–402 (2019).
- Watanabe, J. et al. Indocyanine green fluorescence imaging to reduce the risk of anastomotic leakage in laparoscopic low anterior resection for rectal cancer: a propensity score-matched cohort study. Surg Endosc34, 202–208 (2020).
- Kim, J. C., Lee, J. L. & Park, S. H. Interpretative Guidelines and Possible Indications for Indocyanine Green Fluorescence Imaging in Robot-Assisted Sphincter-Saving Operations. Diseases of the Colon & Rectum 60, 376–384 (2017).
- Nagar, H. et al.Sentinel node biopsy for diagnosis of lymph node involvement in endometrial cancer. Cochrane Database of Systematic Reviews 2021, (2021).
- Baeten, I. G. T. et al.Indocyanine green versus technetium‐99m with blue dye for sentinel lymph node detection in early‐stage cervical cancer: A systematic review and meta‐analysis. Cancer Reports(2021) doi:10.1002/cnr2.1401.
- Buda, A. et al.Real-Time Fluorescent Sentinel Lymph Node Mapping with Indocyanine Green in Women with Previous Conization Undergoing Laparoscopic Surgery for Early Invasive Cervical Cancer: Comparison with Radiotracer ±Blue Dye. Journal of Minimally Invasive Gynecology 25, 455–460 (2018).
- Buda, A. et al.From Conventional Radiotracer Tc-99m with Blue Dye to Indocyanine Green Fluorescence: A Comparison of Methods Towards Optimization of Sentinel Lymph Node Mapping in Early Stage Cervical Cancer for a Laparoscopic Approach. Ann Surg Oncol 23, 2959–2965 (2016).
- Di Martino, G. et al.Indocyanine Green versus Radiotracer with or without Blue Dye for Sentinel Lymph Node Mapping in Stage >IB1 Cervical Cancer (>2cm). Journal of Minimally Invasive Gynecology 24, 954–959 (2017).
- Ballardini, B. et al. The indocyanine green method is equivalent to the 99mTc-labeled radiotracer method for identifying the sentinel node in breast cancer: A concordance and validation study. European Journal of Surgical Oncology (EJSO) 39, 1332–1336 (2013).
- He, K. et al.Comparison between the indocyanine green fluorescence and blue dye methods for sentinel lymph node biopsy using novel fluorescence image-guided resection equipment in different types of hospitals. Translational Research 178, 74–80 (2016).
- Kedrzycki, M. S. et al.Meta-analysis Comparing Fluorescence Imaging with Radioisotope and Blue Dye-Guided Sentinel Node Identification for Breast Cancer Surgery. Ann Surg Oncol 28, 3738–3748 (2021).
- Lin, J. et al.Indocyanine green fluorescence method for sentinel lymph node biopsy in breast cancer. Asian Journal of Surgery 43, 1149–1153 (2020).
- Samorani, D. et al.The use of indocyanine green to detect sentinel nodes in breast cancer: A prospective study. European Journal of Surgical Oncology (EJSO) 41, 64–70 (2015).
- Somashekhar, S. P. et al.Can Low-cost Indo Cyanine Green Florescence Technique for Sentinel Lymph Node Biopsy Replace Dual Dye (Radio-colloid and Blue Dye) Technique in Early Breast Cancer: A Prospective Two-arm Comparative Study. Clinical Breast Cancer 20, e576–e583 (2020).
- van der Vorst, J. R. et al.Randomized Comparison of Near-infrared Fluorescence Imaging Using Indocyanine Green and 99m Technetium With or Without Patent Blue for the Sentinel Lymph Node Procedure in Breast Cancer Patients. Ann Surg Oncol 19, 4104–4111 (2012).
SMACC 2022-32584