Every procedure exposes you and your team to the risk of contamination.

With every day in the operating theatre, surgeons and their teams are facing the risk of a contamination, potentially changing their lives for good.1,2,3
Surgeons and their teams risk getting splashed with blood and other bodily fluids and particles, while performing joint replacements, revisions and other orthopaedic surgeries.2 Transmission of HIV, Hepatitis B and Hepatitis C can all occur through exposure to blood.3
It can take only one drop to get contaminated.3
Orthopaedic surgeons get splashed with an average of 203 blood and fat spots during hip and knee arthroplasties.2
With an average exposure of 203 blood and fat spots with each procedure – and each of these spots potentially causing a contamination - the importance of having a sufficient barrier between surgeon and the surgical site becomes hard to argue.2
.

*In a 30 year career
Some risks are not worth taking.
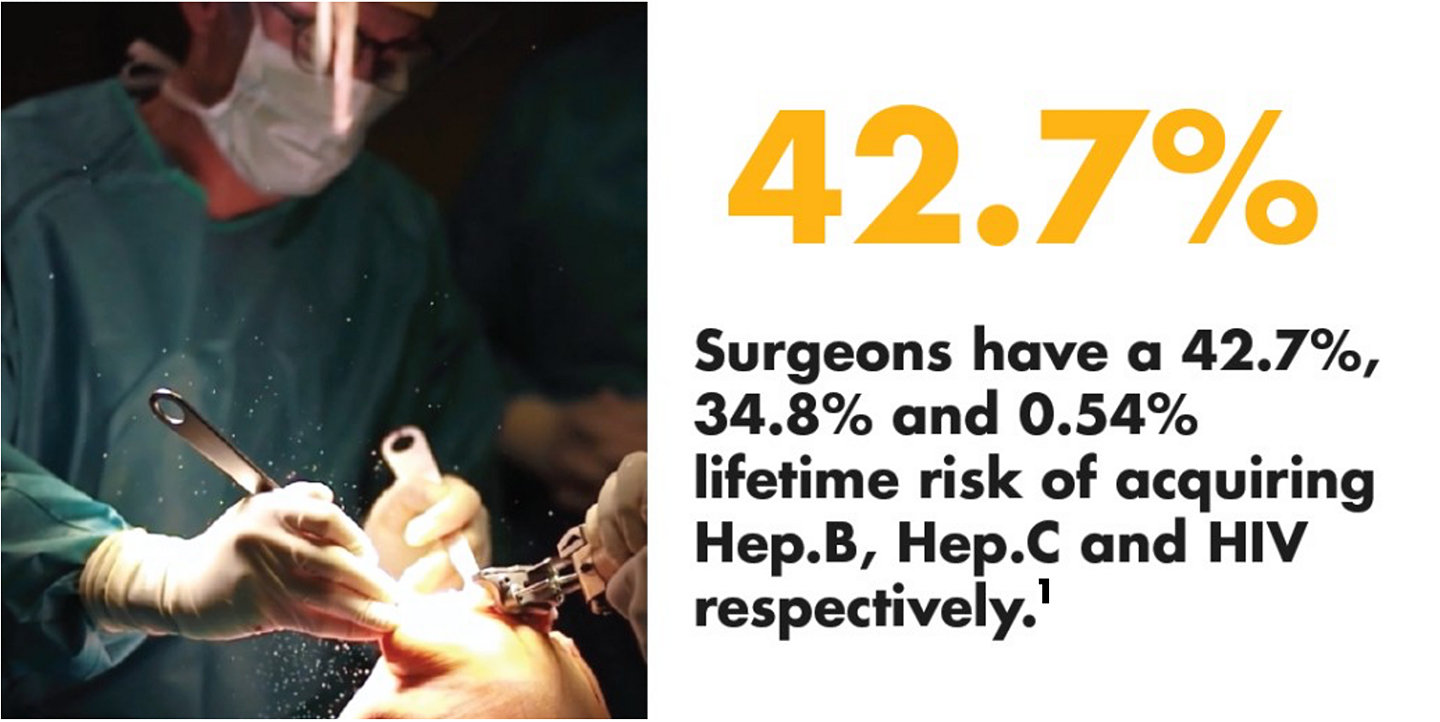
In the majority (83%) of tested procedures, the surgeon's face shield is covered with patient blood, tissue, or bone burr dust.4 Surgeons have a 42.7% risk of acquiring Hepatitis B and a 34.8% risk of acquiring Hepatitis C in a 30 year career.1
Did you know surgical masks may have up to 50% leakage?3
Even when wearing a mask or visor, exposure to blood and bodily fluids during surgery can still result in a surgeon’s contaminated. In 30% of tested cases the surgeon’s conjunctiva is contaminated, despite wearing abovementioned protection.4

.
A mask is not enough.7
Protect yourself. Protect your team.
Besides the impact on the surgeon, a study shows that the use of power tools frequently leads to contamination of all operating theatre personnel in the room, and increases the risk of surface contamination in the operating theatre.5
A contamination might not end with you. It is an unwelcome house guest.

Are the risks you take at work
coming home with you?
Your patients may carry an infectious disease without you even knowing it, putting you at a potential risk of getting contaminated.4,6

Let's rethink
infection control.
”The type of surgery we do will always involve splashes and stains, but we can reduce the risk we face in each surgery, in each patient.”
Dr Revenga - Orthopaedic and Trauma Surgeon*

smacc 2021 29845
References:
1. Pietrabissa A, Merigliano, S., Montorsi M., Poggioli. G, M.D., Stella, M, Borzomati D., Ciferri E., Rossi G., Doglietto, G. (1997) - Reducing the occupational risk of infections for the surgeon: multicentric national survey on more than 15.000 surgical procedures. World Journal of Surgery, 21(6), pp.573-578 | 2. Singh. (2006.). Risk of conjunctival contamination in total joint arthroplasty. Journal of Hospital Infection ,63, 275-280 | 3. Wong, K., & Leung, K. (2004). Transmission and prevention of occupational infections in orthopaedic surgeons. The Journal of bone and joint surgery American, 86-A (5), 1065-76.| 4. Mansour, A., Even, J., Phillips, S., & Halpern, J. (2009). Eye protection in orthopaedic surgery. An in vitro study of various forms of eye protection and their effectiveness. The Journal of bone and joint surgery American volume, 91 (5), 1050-4.| 5. Nogler M, Lass-Florl C, Wimmer C, Bach C, Kaufmann C, Ogon M (2001). Aerosols produced by high-speed cutters in cervical spine surgery: extent of environmental contamination. Eur Spine J 10(4), 274–277. https://doi.org/10.1007/s005860100310 26. | 6. Nogler M, Lass-Florl C, Wimmer C, Mayr E, Bach C, Ogon M (2003). Contamination during removal of cement in revision hip arthroplasty. A cadaver study using ultrasound and highspeed cutters. J Bone Joint Surg Br 85(3):436–439. | 7. "ECDC Technical Report (2020). Safe Use of PPE in Treatment of Infectious Diseases of High Consequence. Retrieved on July 15, 2020. https://www.ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/safe-use-of-ppe.pdf”Intended for the use of Healthcare Professionals only
*Dr. Revenga is a paid consultant of Stryker. The opinions expressed herein are the opinions of Dr. Revenga and not necessarily those of Stryker. Individual experiences may vary.All opinions expressed in this blog are solely and exclusively from Dr. Revenga and do not represent Stryker's.
